The journey toward autologous stem cell transplant or therapy begins with a comprehensive consultation.
Send us all your questions or requests, and our expert team will assist you.

This initial step is crucial for establishing a baseline of the patient’s health.
The medical team reviews the patient’s complete medical history, including past surgeries and chronic conditions. Understanding the trajectory of the current ailment is vital.
Lifestyle factors such as smoking, diet, and physical activity levels are also assessed. These factors can significantly influence the quality of the patient’s own cells.

Before any procedure can take place, rigorous laboratory testing is mandatory. These tests ensure that the patient is a safe candidate for the procedure.
Blood panels are performed to screen for infectious diseases and assess organ function. It is essential to rule out active infections that could complicate the therapy.
Specific markers related to the condition being treated are also measured. This provides a quantitative baseline for later measuring the treatment’s success.

Visualizing the area of injury or disease is a cornerstone of the evaluation process. Advanced imaging techniques provide a roadmap for the stem cell treatment.
MRI scans are frequently used to assess soft tissue damage in orthopedics and neurology. They reveal the extent of cartilage loss or nerve damage.
X-rays and CT scans may be utilized for bone structure analysis. These images help the physician plan the precise delivery of the cells.
Not every patient is a suitable candidate for stem cell therapy. Strict eligibility criteria are maintained to ensure safety and maximize the probability of success.
Patients with active cancer are generally excluded due to the risk of cell proliferation. Similarly, those with severe active infections must be treated for the disease first.
The severity of the condition also plays a role. In some end-stage conditions, the tissue may be too damaged to respond to regenerative therapies.

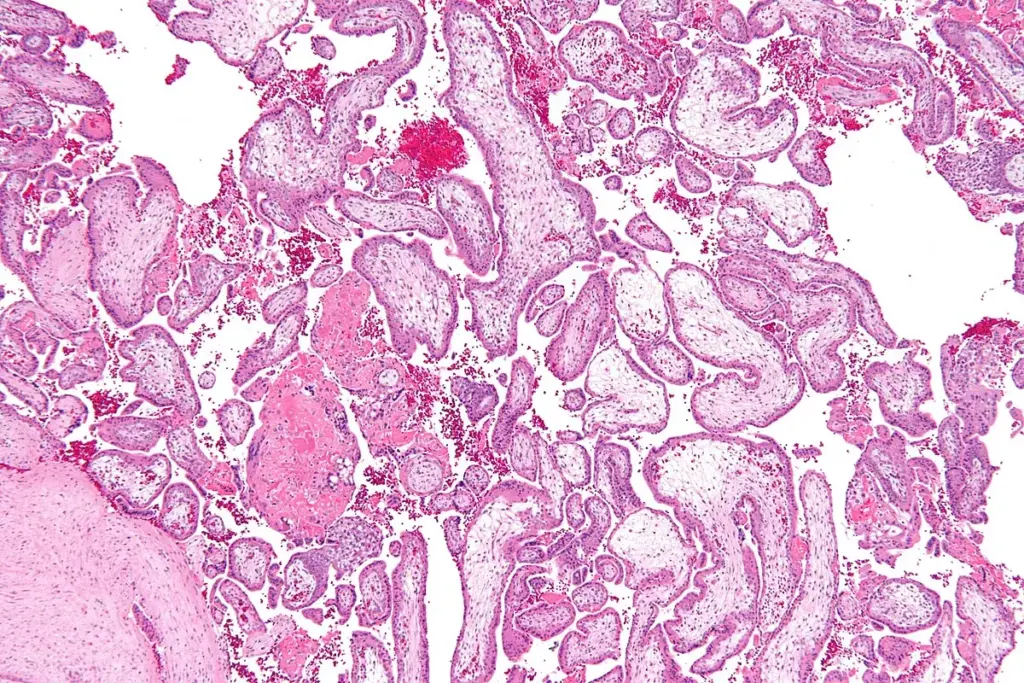
For autologous procedures, the quality of the patient’s own tissue is paramount. The physician evaluates whether the bone marrow or adipose tissue is suitable for harvesting.
Age and chronic illness can affect the potency of stem cells. In some cases, preparatory protocols may be recommended to improve the body’s internal environment before harvesting.
This evaluation determines the best site for collection. The goal is to obtain the highest concentration of viable mesenchymal cells.
In certain complex cases, genetic testing may be incorporated into the evaluation. This is particularly relevant for conditions with a hereditary component.
Understanding the genetic drivers of a disease can help tailor treatment. It helps in predicting how the body might respond to the therapy.
Stem cell research suggests that genetic markers can influence the homing and differentiation capacity of the cells. This adds a layer of personalization to the treatment.
Send us all your questions or requests, and our expert team will assist you.
Since the procedure involves anesthesia or sedation, the heart and lungs must be healthy enough to undergo the process. This is standard preoperative clearance.
An ECG is performed to check the heart’s electrical activity. For patients with a history of heart disease, a cardiologist’s consultation may be required.
Pulmonary function tests may be conducted for patients with respiratory issues. Ensuring stable oxygenation is critical for cell survival post-transplant.
Regenerative medicine is multidisciplinary. The evaluation often involves input from various specialists to ensure a holistic approach.
An orthopedic surgeon will evaluate joint issues, while a neurologist assesses nervous system conditions. This collaboration ensures the diagnosis is accurate.
These specialists confirm that standard treatments have been considered. Stem cell treatment is often positioned as an option when conservative measures have plateaued.
A critical part of the evaluation is ensuring the patient fully understands the procedure. Transparency about the investigational nature of some applications is maintained.
The physician explains the difference between approved indications and off-label uses. The potential risks and benefits are discussed in detail.
Informed consent is a process, not just a signature. It involves a dialogue in which the patient can ask questions about stem cell patches or injection methods.
Once eligibility is confirmed, the preparation for the harvest begins. Patients are given specific instructions to optimize their bodies for the procedure.
Hydration is emphasized to ensure adequate blood volume and tissue quality. Anti-inflammatory medications that might interfere with platelet function are often paused.
Nutrition plays a role; a diet rich in antioxidants is encouraged. The goal is to create the most favorable internal environment for cell collection.
To measure success objectively, quantifiable baselines must be recorded. Subjective pain scores are essential, but objective data are preferred.
Range-of-motion measurements are taken for orthopedic patients. Walking distance or grip strength may be measured in patients with neurological conditions.
These metrics are re-evaluated at specific intervals during follow-up. This data drives the broader stem cell research field forward.
Chronic illness takes a toll on mental health. Assessing the patient’s psychological state is part of the holistic evaluation.
A positive mindset can influence recovery outcomes. Patients are evaluated for signs of depression or anxiety that might hinder rehabilitation.
Social support systems are also checked. Having a caregiver or family member to assist during the recovery phase is highly beneficial.
In complex medical scenarios, seeking a second opinion is encouraged. The medical team reviews outside records to ensure nothing has been missed.
This collaborative approach builds trust. It confirms that the diagnosis is robust and the proposed stem cell therapy is the most appropriate path.
Hospital review boards may discuss complex cases. This ensures that the decision to proceed is backed by collective expertise.
The final step before scheduling is a final safety check for contraindications. These are specific conditions that make the procedure unsafe.
Pregnancy is a strict contraindication for these procedures. Severe anemia or bleeding disorders also require management before proceeding.
Allergies to anesthetics or reagents used in cell processing are identified. Safety is the absolute priority.
Standard tests include complete blood panels, infectious disease screening, metabolic profiles, and imaging (MRI or X-ray) specific to the injury site.
Certain medications, especially anti-inflammatories and blood thinners, can interfere with the harvesting process and the effectiveness of the platelets or cells.
Doctors evaluate the cell count and viability during the laboratory processing phase immediately after harvesting bone marrow or fat tissue.
No, active infections must be fully resolved before the procedure to prevent spreading bacteria and to ensure the immune system is stable.
Genetic testing is not routine for all orthopedic cases, but it may be utilized for complex autoimmune or neurological conditions to tailor the therapy.





Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)